Private health insurers use AI to approve or deny care. Soon Medicare will, too.
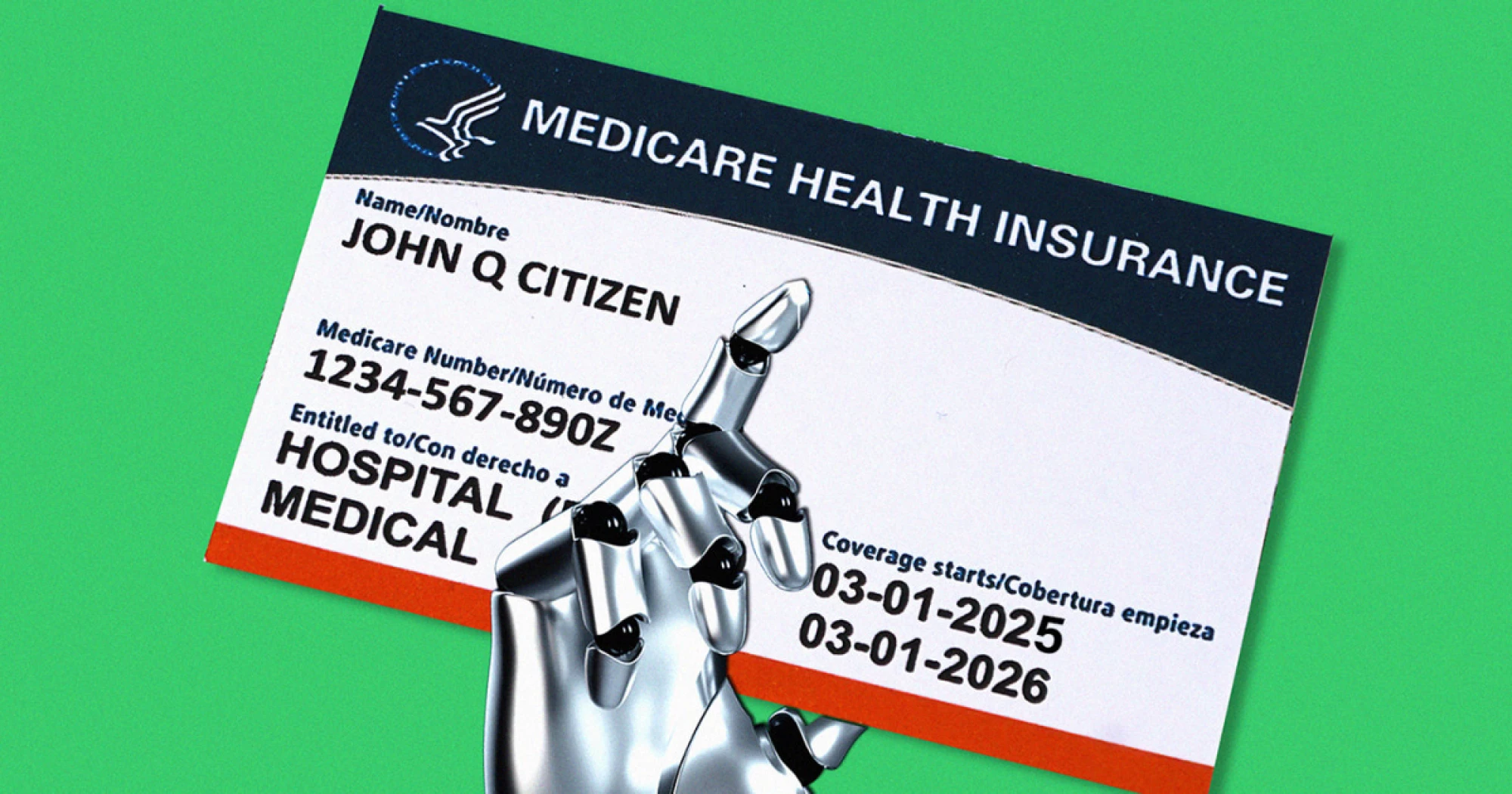
Taking a page from the private insurance industry’s playbook, Medicare will launch an AI program for prior authorizations.
Taking a page from the private insurance industry’s playbook, the Trump administration will launch a program next year to find out how much money an artificial intelligence algorithm could save the federal government by denying care to Medicare patients.
The pilot program, designed to weed out wasteful, “low-value” services, amounts to a federal expansion of an unpopular process called prior authorization, which requires patients or someone on their medical team to seek insurance approval before proceeding with certain procedures, tests, and prescriptions. It will affect Medicare patients, and the doctors and hospitals who care for them, in Arizona, Ohio, Oklahoma, New Jersey, Texas, and Washington, starting Jan. 1 and running through 2031.
The move has raised eyebrows among politicians and policy experts. The traditional version of Medicare, which covers adults 65 and older and some people with disabilities, has mostly eschewed prior authorization. Still, it is widely used by private insurers, especially in the Medicare Advantage market.
And the timing was surprising: The pilot was announced in late June, just days after the Trump administration unveiled a voluntary effort by private health insurers to revamp and reduce their own use of prior authorization, which causes care to be “significantly delayed,” said Dr. Mehmet Oz, administrator of the Centers for Medicare & Medicaid Services.
“It erodes public trust in the health care system,” Oz told the media. “It’s something that we can’t tolerate in this administration.”
Rating: 5