Insurance denied an $800,000 drug twice. A state-run outside panel helped a North Carolina teen get it.
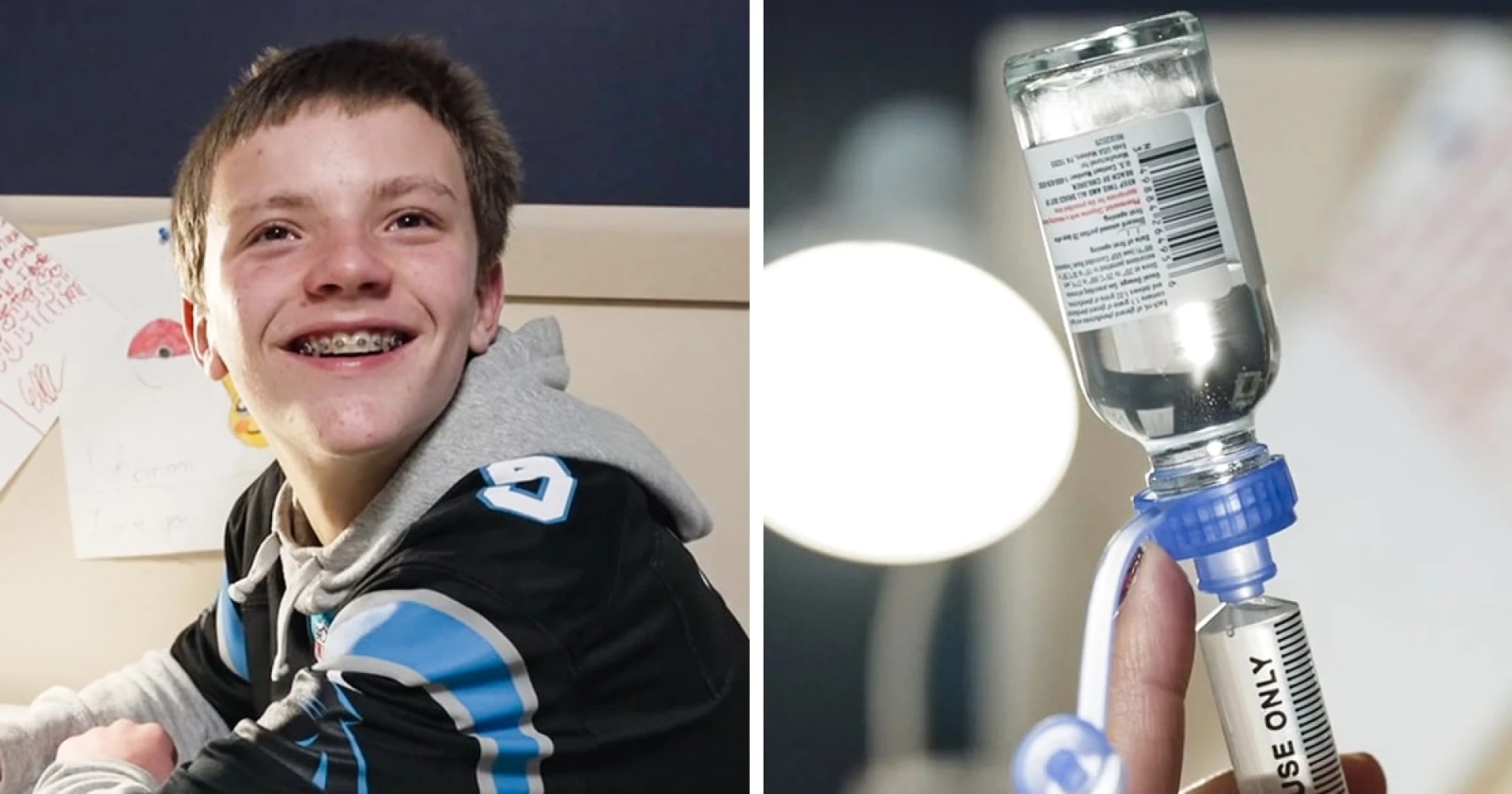
When insurance twice refused to cover a nearly $800,000-a-year drug that Paxton Pope’s doctor believed could dramatically reduce his frequent seizures, his family initially braced for a serious medical setback.
When insurance twice refused to cover a nearly $800,000-a-year drug that Paxton Pope’s doctor believed could dramatically reduce his frequent seizures, his family initially braced for a serious medical setback.
Then the Popes, of Davidson, North Carolina, learned about a little-known provision in the Affordable Care Act that allows asking an outside state-run panel to review the insurer’s decision — a move that led to the denial ultimately being overturned.
In the few months since then, access to the drug has already transformed the 13-year-old’s life, according to his mother, Maggie Pope. Paxton went from as many as 12 seizures an hour to about eight a day, she said, and he’s regaining skills he had started to lose, like holding conversations and telling them what he’s reading in school. For the first time, he’s able to play on his school’s flag football team.
“I was just over the moon,” Maggie Pope said. “I looked over at him, and he was just smiling. I said, ‘Paxton, did you know you were having less seizures?’ And he just kind of shook his head, ‘Yeah.’”
Rating: 5